· Mayank Kashyap · 7 min read
Stomach
the stomach is a J-shaped dilated portion of the gastrointestinal tract that serves as a reservoir for food and initiates the digestive process through mechanical and chemical means.
Introduction to the Stomach
According to Love and Bailey’s “A Short Practice of Surgery”, the stomach is a J-shaped dilated portion of the gastrointestinal tract that serves as a reservoir for food and initiates the digestive process through mechanical and chemical means.
Clinical Significance
Primary organ for food storage and initial digestion
Site of common surgical conditions like PUD and gastric cancer
Gastric cancer is the 5th most common cancer worldwide
Peptic ulcer disease affects 4-10% of population
Major site for bariatric surgical procedures
Surgical Anatomy of the Stomach
Gross Anatomy and Relations
| Part | Location | Relations |
|---|---|---|
| Cardia | T11 level, left of midline | Left lobe of liver anteriorly, diaphragm posteriorly |
| Fundus | Superior to cardia, dome-shaped | Left dome of diaphragm, spleen laterally |
| Body | Between fundus and antrum | Anterior: Left lobe liver, Posterior: Pancreas, spleen |
| Antrum | Distal third, prepyloric region | Gallbladder anteriorly, pancreas posteriorly |
| Pylorus | Gastroduodenal junction | First part of duodenum, portal vein posteriorly |
Peritoneal Attachments
| Ligament | Attachment | Contents | Clinical Significance |
|---|---|---|---|
| Gastrohepatic | Lesser curvature to liver | Left gastric artery, coronary vein, lymph nodes | Access to lesser sac, contains aberrant left hepatic artery |
| Gastrosplenic | Greater curvature to spleen | Short gastric vessels, left gastroepiploic vessels | Risk of splenic injury during gastrectomy |
| Gastrocolic | Greater curvature to transverse colon | Right and left gastroepiploic vessels | Access to lesser sac, important in gastric mobilization |
| Gastrophrenic | Fundus to diaphragm | Peritoneum only | Mobilization for fundoplication |
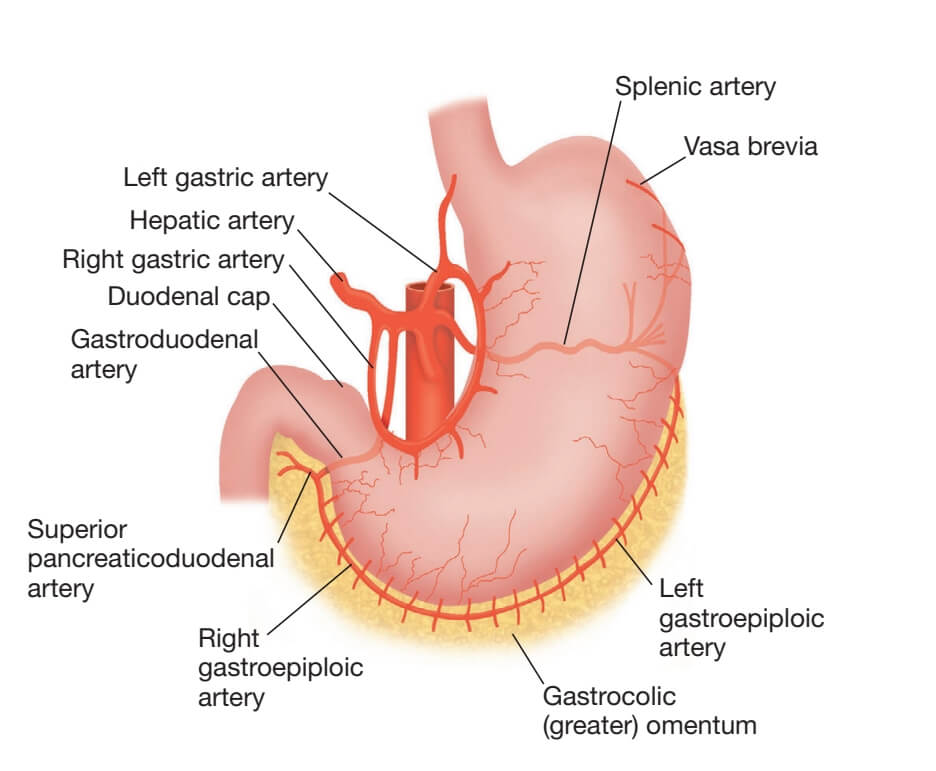
Blood Supply
| Artery | Origin | Distribution | Surgical Importance |
|---|---|---|---|
| Left Gastric | Celiac trunk | Lesser curvature, cardia, lower esophagus | First vessel ligated in gastrectomy, supplies anastomosis |
| Right Gastric | Common hepatic artery | Distal lesser curvature, pylorus | Preserved in pylorus-preserving procedures |
| Right Gastroepiploic | Gastroduodenal artery | Greater curvature, body, antrum | Major blood supply for gastric conduit |
| Left Gastroepiploic | Splenic artery | Upper greater curvature, fundus | Ligated during splenectomy, gastrectomy |
| Short Gastric | Splenic artery | Fundus of stomach | Ligated during fundoplication, splenectomy |
| Posterior Gastric | Splenic artery | Posterior wall of fundus | Present in 60% of individuals |
Venous Drainage
Right and Left Gastric veins: Portal vein
Right Gastroepiploic vein: Superior mesenteric vein
Left Gastroepiploic and Short Gastric veins: Splenic vein
Clinical significance: Portal hypertension → gastric varices
Lymphatic Drainage
| Zone | Primary Drainage | Secondary Drainage | Clinical Significance |
|---|---|---|---|
| Lower esophagus/cardia | Paracardial nodes | Left gastric, celiac nodes | Early spread of proximal gastric cancer |
| Lesser curvature | Left and right gastric nodes | Celiac nodes | Standard D2 lymphadenectomy includes these |
| Greater curvature (right) | Right gastroepiploic nodes | Subpyloric, hepatic nodes | Important in antral cancers |
| Greater curvature (left) | Left gastroepiploic nodes | Pancreaticosplenic nodes | Involved in fundic cancers |
| Pylorus | Supra- and subpyloric nodes | Hepatic, celiac nodes | Early nodal spread in distal cancers |
Nerve Supply
| Nerve | Origin | Function | Clinical Significance |
|---|---|---|---|
| Anterior Vagal Trunk | Left vagus nerve | Motor to stomach, pyloric relaxation, hepatic branch | Truncal vagotomy for PUD, highly selective preserves branches |
| Posterior Vagal Trunk | Right vagus nerve | Motor to stomach, celiac branch to intestine | Truncal vagotomy, must preserve celiac branch |
| Sympathetic Nerves | T6-T9 via greater splanchnic nerve | Vasomotor, inhibitory to motility, pain sensation | Pain referral to epigastrium |
Histology of Gastric Wall
| Layer | Composition | Function |
|---|---|---|
| Mucosa | Surface epithelium, lamina propria, muscularis mucosae | Secretion, absorption, barrier function |
| Submucosa | Loose connective tissue, vessels, nerves (Meissner’s plexus) | Nutrition, neural regulation |
| Muscularis Propria | Inner oblique, middle circular, outer longitudinal layers | Mixing and propulsion of gastric contents |
| Serosa | Visceral peritoneum | Reduces friction, contains blood vessels |
Gastric Physiology
Gastric Secretions
| Cell Type | Location | Secretion | Function |
|---|---|---|---|
| Parietal (Oxyntic) Cells | Body and fundus | Hydrochloric acid, intrinsic factor | Acidification, protein denaturation, B12 absorption |
| Chief (Zymogenic) Cells | Body and fundus | Pepsinogen, gastric lipase | Protein and fat digestion |
| Mucous Cells | Throughout stomach | Mucus, bicarbonate | Protection against acid and pepsin |
| G Cells | Antrum | Gastrin | Stimulates acid secretion, mucosal growth |
| D Cells | Antrum and body | Somatostatin | Inhibits acid secretion |
| Enterochromaffin-like (ECL) Cells | Body and fundus | Histamine | Stimulates acid secretion |
Phases of Gastric Secretion
| Phase | Stimulus | Mechanism | % of Total Secretion |
|---|---|---|---|
| Cephalic | Sight, smell, taste of food | Vagal stimulation via hypothalamus | 30% |
| Gastric | Gastric distension, peptides | Local reflexes, gastrin release | 60% |
| Intestinal | Chyme in duodenum | Enterogastrone release (secretin, CCK) | 10% |
Gastric Motility
Receptive relaxation: Fundic relaxation to accommodate food
Mixing waves: Peristaltic contractions in body (3/minute)
Gastric emptying: Regulated by pylorus, duodenal receptors
Factors delaying emptying: Fat, acid, hypertonicity, distension
Normal emptying time: 2-4 hours for mixed meal
Congenital Gastric Disorders
Pyloric Stenosis
| Aspect | Details |
|---|---|
| Incidence | 2-4 per 1000 live births, male:female = 4:1 |
| Pathology | Hypertrophy and hyperplasia of pyloric circular muscle |
| Clinical Features | Non-bilious projectile vomiting at 3-6 weeks, visible peristalsis, palpable olive-shaped mass |
| Diagnosis | Clinical examination, ultrasound (muscle thickness >4mm, length >16mm) |
| Treatment | Ramstedt’s pyloromyotomy (longitudinal division of muscle) |
Other Congenital Anomalies
| Anomaly | Features | Treatment |
|---|---|---|
| Gastric Atresia | Rare, usually prepyloric, associated with polyhydramnios | Resection with gastroduodenostomy |
| Microgastria | Small tubular stomach, associated with malrotation | Gastric augmentation or feeding procedures |
| Gastric Duplication Cysts | Usually along greater curvature, may contain gastric mucosa | Excision if symptomatic |
| Congenital Gastric Volvulus | Organoaxial or mesenteroaxial rotation | Emergency derotation and fixation |
Inflammatory Gastric Disorders
Peptic Ulcer Disease
| Feature | Gastric Ulcer | Duodenal Ulcer |
|---|---|---|
| Location | Lesser curvature, antrum-body junction | First part of duodenum (95%) |
| Age | Older adults (40-70 years) | Younger adults (20-50 years) |
| Pain Pattern | Soon after eating, may be worsened by food | 2-3 hours after meals, relieved by food |
| Acid Secretion | Normal or low | High |
| H. pylori Association | 70-80% | 90-95% |
| Malignancy Risk | 2-4% | Virtually nil |
Complications of Peptic Ulcer Disease
| Complication | Incidence | Clinical Features | Management |
|---|---|---|---|
| Hemorrhage | 15-20% of PUD patients | Hematemesis, melena, shock | Resuscitation, endoscopy (injection, clipping), surgery if persistent |
| Perforation | 5-10% of PUD patients | Sudden severe epigastric pain, board-like rigidity, air under diaphragm | Resuscitation, antibiotics, surgery (oversewing + patch, resection) |
| Obstruction | 2-5% of PUD patients | Vomiting, dehydration, metabolic alkalosis, succussion splash | NG decompression, IV fluids, PPI, endoscopic dilatation or surgery |
| Penetration | 1-2% of PUD patients | Back pain (pancreas), jaundice (bile duct), change in pain pattern | Medical treatment, surgery if medical failure |
Gastritis Classification
| Type | Etiology | Location | Clinical Features |
|---|---|---|---|
| Acute Erosive | NSAIDs, alcohol, stress, burns (Curling’s), CNS injury (Cushing’s) | Diffuse, multiple erosions | Bleeding, epigastric pain |
| Chronic Superficial | H. pylori, autoimmune, bile reflux | Antrum (H. pylori), body (autoimmune) | Dyspepsia, risk of atrophy and cancer |
| Atrophic Gastritis | Long-standing H. pylori, autoimmune (pernicious anemia) | Body and fundus | Achlorhydria, B12 deficiency, increased cancer risk |
Helicobacter pylori Infection
Prevalence: 50% of world population, higher in developing countries
Transmission: Fecal-oral, oral-oral, contaminated water
Pathogenesis: Urease production, VacA and CagA toxins, inflammation
Diagnosis:
Non-invasive: Urea breath test, stool antigen, serology
Invasive: Rapid urease test, histology, culture
Treatment: Triple therapy (PPI + clarithromycin + amoxicillin/metronidazole)
Gastric Tumors
Benign Gastric Tumors
| Tumor Type | Frequency | Features | Management |
|---|---|---|---|
| Gastric Adenoma | Most common benign epithelial tumor | Usually in antrum, premalignant (30-40% risk) | Endoscopic resection, surveillance |
| Gastrointestinal Stromal Tumor (GIST) | Most common benign mesenchymal tumor | Submucosal, CD117 positive, variable malignant potential | Local excision with clear margins |
| Leiomyoma | Common benign smooth muscle tumor | Usually asymptomatic, may ulcerate and bleed | Excision if symptomatic or growing |
| Lipoma | Rare | Submucosal, yellow color on endoscopy | Excision if symptomatic |
Gastric Carcinoma
| Feature | Intestinal Type | Diffuse Type |
|---|---|---|
| Incidence | Decreasing worldwide | Stable or increasing |
| Age | Older adults (50-70 years) | Younger adults (30-50 years) |
| Geography | High in Japan, China, South America | Similar worldwide |
| Risk Factors | H. pylori, atrophic gastritis, dietary nitrites, smoking | Genetic (E-cadherin mutation), blood group A |
| Pathology | Gland formation, intestinal metaplasia | Signet ring cells, limits plastica |
| Location | Antrum (50%), lesser curvature | Body and fundus, diffuse involvement |
| Prognosis | Better, if detected early | Poor, early spread |
Staging of Gastric Cancer (TNM 8th Edition)
| Stage | T | N | M | 5-year Survival |
|---|---|---|---|---|
| 0 | Tis | N0 | M0 | >90% |
| IA | T1 | N0 | M0 | 70-80% |
| IB | T2 | N0 | M0 | 60-70% |
| IIA | T3 | N0 | M0 | 40-50% |
| IIB | T1-2 | N1 | M0 | 30-40% |
| IIIA | T3-4a | N1 | M0 | 20-30% |
| IIIB | T2-3 | N2 | M0 | 10-20% |
| IIIC | T4a | N3 | M0 | 5-10% |
| IV | Any T | Any N | M1 | <5% |
Other Malignant Tumors
| Tumor Type | Frequency | Features | Treatment |
|---|---|---|---|
| Gastric Lymphoma | 5% of gastric malignancies | Usually NHL, MALT type associated with H. pylori | H. pylori eradication, chemotherapy, radiotherapy |
| GIST | 1-2% of gastric malignancies | CD117 positive, variable malignant potential | Surgery, imatinib for metastatic disease |
| Carcinoid Tumors | Rare | Type I: Associated with atrophic gastritis, Type II: ZES, Type III: Sporadic | Endoscopic resection, antrectomy, formal resection |
Gastric Surgery
Surgical Procedures for Peptic Ulcer Disease
| Procedure | Technique | Indications | Complications |
|---|---|---|---|
| Truncal Vagotomy + Drainage | Division of main vagal trunks + pyloroplasty/gastrojejunostomy | Elective for DU, not commonly used now | Dumping, diarrhea, gallstones |
| Selective Vagotomy | Preserves hepatic and celiac branches | Historical, rarely used | Less diarrhea than truncal |
| Highly Selective Vagotomy | Denervates corpus and fundus only, preserves antral innervation | Elective DU without obstruction | Lower complication rate, higher recurrence |
| Vagotomy + Antrectomy | Vagotomy + distal 40% gastrectomy | Complicated PUD, gastric outlet obstruction | Dumping, diarrhea, nutritional deficiencies |
Gastric Resection for Cancer
| Procedure | Extent of Resection | Indications | Reconstruction |
|---|---|---|---|
| Distal Gastrectomy | Antrum and pylorus (50-60% stomach) | Distal gastric cancer | Billroth I, Billroth II, Roux-en-Y |
| Total Gastrectomy | Entire stomach, omentum, lymph nodes | Proximal cancer, limits plastica, extensive tumors | Roux-en-Y esophagojejunostomy |
| Proximal Gastrectomy | Cardia and proximal stomach | Early proximal cancers | Esophagogastrostomy |
| Wedged Resection | Local excision of tumor with margin | Early gastric cancer, benign tumors | Primary closure |
Lymph Node Dissection in Gastric Cancer
| Dissection | Nodes Removed | Indications | Survival Benefit |
|---|---|---|---|
| D1 | Perigastric nodes (stations 1-6) | Early gastric cancer (T1) | Standard for early cancer |
| D2 | D1 + nodes along left gastric, common hepatic, splenic arteries, celiac axis | Advanced gastric cancer (T2-4) | Improved survival in experienced centers |
| D3 | D2 + para-aortic nodes | Selected cases in Japan | No proven survival benefit |
Postgastrectomy Syndromes
| Syndrome | Onset | Pathophysiology | Management |
|---|---|---|---|
| Dumping Syndrome | Early (30 min) or late (2-3 hours) | Rapid gastric emptying, hyperosmolar contents | Diet modification, acarbose, somatostatin |
| Afferent Loop Syndrome | Postprandial | Obstruction of afferent limb in Billroth II | Surgical revision to Roux-en-Y |
| Alkaline Reflux Gastritis | Weeks to months | Bile reflux damaging gastric mucosa | Medical therapy, Roux-en-Y conversion |
| Postvagotomy Diarrhea | Variable | Rapid intestinal transit, bile salt malabsorption | Diet, cholestyramine, codeine |
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Gastric Diseases in Love & Bailey’s textbook
American College of Gastroenterology Guidelines
Japanese Gastric Cancer Association Guidelines
European Society for Medical Oncology (ESMO) Guidelines
National Comprehensive Cancer Network (NCCN) Guidelines
Key Learning Points from Love & Bailey
“The stomach, with its complex anatomy and physiology, presents unique surgical challenges. A thorough understanding of gastric blood supply, lymphatic drainage, and nerve supply is essential for safe and effective surgical management of both benign and malignant gastric conditions.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Always test for H. pylori in peptic ulcer disease and gastric lymphoma
Early gastric cancer is often asymptomatic - maintain high index of suspicion
D2 lymphadenectomy improves survival in advanced gastric cancer when performed by experienced surgeons
Postgastrectomy syndromes can significantly impact quality of life
Nutritional support is crucial after major gastric surgery
Multimodal therapy is standard for locally advanced gastric cancer
Regular surveillance endoscopy is needed for high-risk conditions like gastric atrophy and adenomas
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog