· Mayank Kashyap · 7 min read
Hemorrhoids
When these cushions become engorged, prolapsed, or symptomatic, they are referred to as hemorrhoidal disease.
Introduction to Hemorrhoids
According to Love and Bailey’s “A Short Practice of Surgery”, hemorrhoids are vascular cushions located in the anal canal that consist of blood vessels, smooth muscle, and connective tissue. When these cushions become engorged, prolapsed, or symptomatic, they are referred to as hemorrhoidal disease.
Historical Perspective
Term derived from Greek “haima” (blood) and “rhoos” (flowing)
One of the oldest recorded medical conditions - mentioned in Egyptian papyri (1700 BC)
Hippocrates described treatment with cautery
Common condition affecting millions worldwide
Epidemiology
| Population | Prevalence | Remarks |
|---|---|---|
| General Population | 4-5% | Higher in Western countries |
| Age >50 years | 50% | Peak incidence 45-65 years |
| Gender Distribution | Equal M:F | Slightly more common in males |
| Pregnant Women | 25-35% | Usually resolves postpartum |
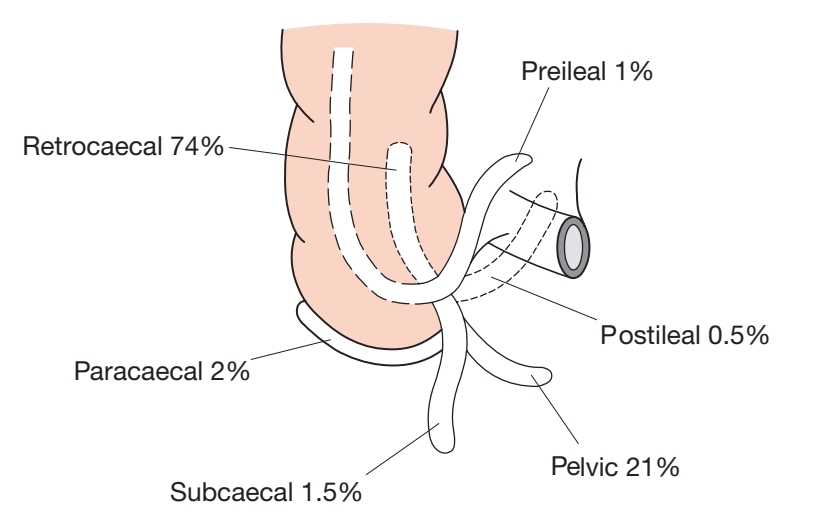
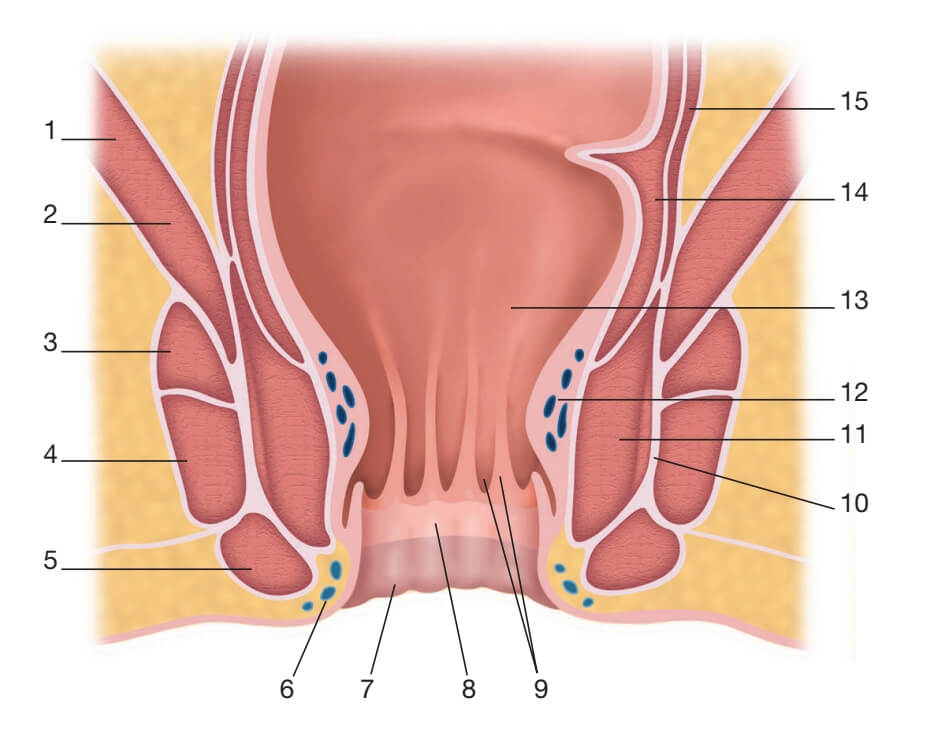
Surgical Anatomy of Hemorrhoids
Anatomy of Anal Canal
| Structure | Length | Features |
|---|---|---|
| Anal Canal | 4 cm (adults) | Extends from anorectal junction to anal verge |
| Dentate Line | Mid-anal canal | Embryological junction between endoderm and ectoderm |
| Anal Columns (Columns of Morgagni) | 6-10 vertical folds | Contain terminal branches of superior rectal artery |
| Anal Valves | At bases of columns | Semilunar folds between columns |
| Anal Crypts | Above valves | Openings of anal glands |
Hemorrhoidal Vascular Cushions
| Cushion | Position | Arterial Supply | Clinical Significance |
|---|---|---|---|
| Left Lateral | 3 o’clock (lithotomy) | Inferior mesenteric → superior rectal artery | Most common site for bleeding |
| Right Anterior | 11 o’clock (lithotomy) | Internal iliac → middle rectal artery | Common in pregnant women |
| Right Posterior | 7 o’clock (lithotomy) | Internal iliac → middle rectal artery | Often associated with prolapse |
Blood Supply
| Artery | Origin | Distribution |
|---|---|---|
| Superior Rectal Artery | Inferior mesenteric artery | Main supply to internal hemorrhoids |
| Middle Rectal Artery | Internal iliac artery | Anastomoses with superior and inferior rectal arteries |
| Inferior Rectal Artery | Internal pudendal artery | Supplies external hemorrhoids and sphincters |
Venous Drainage
Above dentate line: Superior rectal vein → inferior mesenteric vein → portal system
Below dentate line: Inferior rectal vein → internal pudendal vein → internal iliac vein → systemic system
Clinical significance: Portal hypertension can cause hemorrhoids but is not the primary cause
Nerve Supply
| Area | Innervation | Sensation |
|---|---|---|
| Above Dentate Line | Autonomic nerves (sympathetic and parasympathetic) | Visceral pain (dull, poorly localized) |
| Below Dentate Line | Inferior rectal nerves (somatic) | Somatic pain (sharp, well-localized) |
Classification of Hemorrhoids
Anatomical Classification
| Type | Location | Covering | Nerve Supply |
|---|---|---|---|
| Internal Hemorrhoids | Above dentate line | Columnar epithelium | Autonomic (pain insensitive) |
| External Hemorrhoids | Below dentate line | Stratified squamous epithelium | Somatic (pain sensitive) |
| Mixed Hemorrhoids | Above and below dentate line | Both epithelial types | Both autonomic and somatic |
Goligher’s Classification of Internal Hemorrhoids
| Grade | Description | Clinical Features | Treatment Options |
|---|---|---|---|
| First Degree | Bleed but do not prolapse | Bright red bleeding, no prolapse | Diet, fiber, sclerotherapy, banding |
| Second Degree | Prolapse on straining but reduce spontaneously | Prolapse with defecation, spontaneous reduction | Banding, infrared coagulation, hemorrhoidectomy |
| Third Degree | Prolapse and require manual reduction | Prolapse requires manual reduction | Hemorrhoidectomy, stapled hemorrhoidopexy |
| Fourth Degree | Permanently prolapsed and irreducible | Chronic prolapse, may strangulate | Emergency hemorrhoidectomy if strangulated |
External Hemorrhoid Types
| Type | Features | Management |
|---|---|---|
| Cutaneous Tags | Skin folds, usually asymptomatic | Reassurance, excision if symptomatic |
| Thrombosed External Hemorrhoid | Acute painful swelling due to thrombosis | Evacuation if <72 hours, conservative if >72 hours |
| Chronic External Hemorrhoid | Persistent swelling, irritation | Excision if symptomatic |
Etiology and Pathophysiology
Pathophysiological Theories
| Theory | Proponent | Mechanism | Evidence |
|---|---|---|---|
| Varicose Vein Theory | Ancient theory | Dilatation of hemorrhoidal veins | Weak evidence - hemorrhoids are vascular cushions, not varicosities |
| Sliding Anal Lining Theory | Parks (1956) | Weakening of supporting tissues leads to prolapse | Currently accepted theory |
| Vascular Hyperplasia Theory | Thomson (1975) | Engorgement of vascular cushions | Hemorrhoids contain arteriovenous communications |
Risk Factors
| Risk Factor | Mechanism | Strength of Association |
|---|---|---|
| Chronic Constipation | Increased straining, raised intra-abdominal pressure | Strong |
| Pregnancy | Mechanical pressure, hormonal changes | Strong |
| Aging | Weakening of connective tissue supports | Strong |
| Prolonged Sitting | Increased venous pressure in pelvis | Moderate |
| Heavy Lifting | Increased intra-abdominal pressure | Moderate |
| Obesity | Increased intra-abdominal pressure | Moderate |
| Low Fiber Diet | Leads to constipation and straining | Strong |
| Family History | Genetic predisposition | Weak to moderate |
| Portal Hypertension | Increased venous pressure | Weak (not primary cause) |
Pathological Changes
Degeneration of supporting tissues: Treitz’s muscle and connective tissue
Vascular changes: Dilatation of venules, arteriolar hypertrophy
Inflammation: Secondary to trauma, thrombosis, or infection
Fibrosis: Chronic inflammation leads to fibrosis
Thrombosis: Particularly in external hemorrhoids
Clinical Features
Symptoms of Hemorrhoids
| Symptom | Internal Hemorrhoids | External Hemorrhoids | Clinical Significance |
|---|---|---|---|
| Bleeding | Common (bright red, on toilet paper or dripping) | Rare (only if ulcerated) | Most common presenting symptom |
| Prolapse | Grades II-IV | Not applicable | Indicates more advanced disease |
| Pain | Rare (unless thrombosed or strangulated) | Common (especially when thrombosed) | Pain suggests complication or alternative diagnosis |
| Pruritus | Common (due to mucus secretion) | Less common | Due to moisture and irritation |
| Soiling | Common (incomplete closure of anal canal) | Less common | Due to prolapse interfering with closure |
Special Clinical Scenarios
Thrombosed External Hemorrhoid
Presentation: Acute, severe perianal pain with sudden onset
Examination: Tender, bluish, swollen lump at anal verge
Natural history: Pain peaks at 48 hours, resolves in 7-10 days
Treatment: Evacuation if <72 hours, conservative if >72 hours
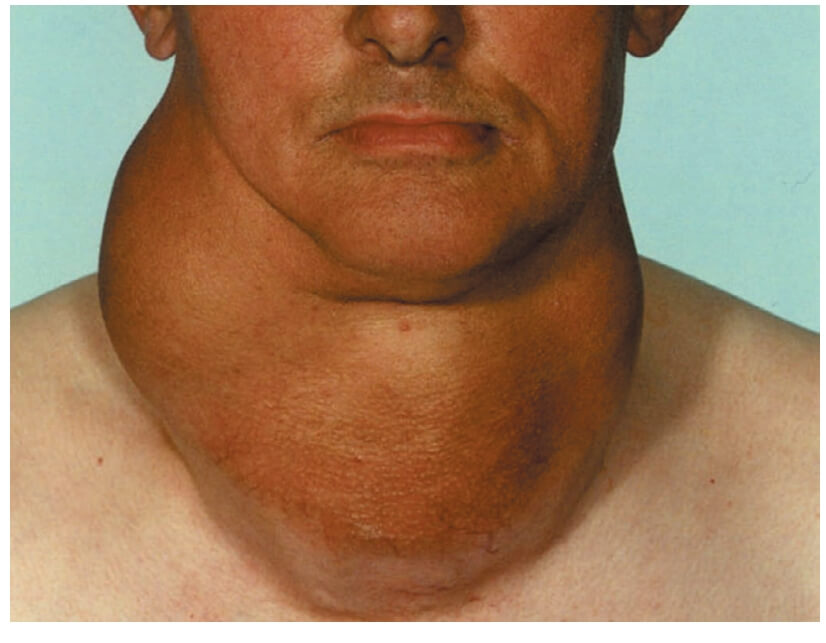
Strangulated Hemorrhoids
Pathophysiology: Prolapsed hemorrhoids with compromised blood supply
Clinical features: Severe pain, swelling, tenderness, possible necrosis
Treatment: Emergency hemorrhoidectomy
Complications: Gangrene, sepsis, portal pyaemia (rare)
Hemorrhoids in Pregnancy
Incidence: 25-35% of pregnancies
Causes: Mechanical pressure, hormonal changes, constipation
Management: Conservative (fiber, stool softeners, topical treatments)
Surgery: Reserved for severe complications
Diagnosis of Hemorrhoids
Clinical Assessment
| Examination | Technique | Findings |
|---|---|---|
| Inspection | Patient in left lateral position, examine perianal area | External hemorrhoids, skin tags, prolapse, excoriation |
| Digital Rectal Examination | Lubricated gloved finger, assess tone, masses, tenderness | Internal hemorrhoids usually not palpable unless thrombosed |
| Proctoscopy | Patient straining, proctoscope inserted and slowly withdrawn | Internal hemorrhoids bulge into lumen at 3,7,11 o’clock |
| Sigmoidoscopy/Colonoscopy | If bleeding or age >50 years, to exclude other pathology | Rule out colorectal cancer, inflammatory bowel disease |
Differential Diagnosis
| Condition | Distinguishing Features |
|---|---|
| Anal Fissure | Sharp pain with defecation, sentinel pile, visible fissure |
| Perianal Abscess/Fistula | Pain, swelling, discharge, fever, external opening |
| Rectal Prolapse | Concentric mucosal folds, complete thickness prolapse |
| Anal Cancer | Ulcerated, indurated lesion, bleeding, pain |
| Condylomata Acuminata | Wart-like lesions, multiple, may be extensive |
| Inflammatory Bowel Disease | Diarrhea, mucus, systemic symptoms, perianal skin tags |
| Rectal Polyp/Cancer | Altered bowel habit, weight loss, anemia, mass on examination |
Investigations
| Investigation | Indications | Findings |
|---|---|---|
| Complete Blood Count | Significant bleeding, anemia suspected | Anemia (microcytic if chronic bleeding) |
| Coagulation Profile | Bleeding diathesis suspected | Prolonged PT/PTT if coagulopathy |
| Flexible Sigmoidoscopy | Age <50 years with bleeding, no alarm features | Exclude distal colorectal pathology |
| Colonoscopy | Age >50 years, family history, alarm features | Exclude colorectal cancer, polyps, IBD |
| Anorectal Physiology | Incontinence, prior anal surgery | Assess sphincter function |
Treatment of Hemorrhoids
Conservative Management
| Modality | Mechanism | Indications | Effectiveness |
|---|---|---|---|
| Dietary Modification | Increase fiber, fluids to soften stools | All grades, first-line treatment | 50% reduction in symptoms |
| Topical Treatments | Local anesthesia, anti-inflammatory, vasoconstriction | Symptomatic relief | Good for symptom control |
| Sitz Baths | Warm water improves hygiene, reduces sphincter spasm | Pain, irritation, postoperatively | Good symptomatic relief |
| Stool Softeners | Reduce straining | Constipation, postoperative | Effective for constipation |
Office-Based Procedures
| Procedure | Mechanism | Indications | Success Rate | Complications |
|---|---|---|---|---|
| Rubber Band Ligation | Ischemic necrosis of hemorrhoid | Grade I-III hemorrhoids | 70-80% | Pain, bleeding, thrombosis |
| Sclerotherapy | Fibrosis and fixation of mucosa | Grade I-II hemorrhoids | 60-70% | Ulceration, prostatitis, impotence (rare) |
| Infrared Coagulation | Coagulation and fibrosis | Grade I-II hemorrhoids | 60-70% | Mild pain, bleeding |
| Cryotherapy | Tissue destruction by freezing | Historical, rarely used now | Variable | Profuse discharge, pain |
Surgical Procedures
| Procedure | Technique | Indications | Advantages | Disadvantages |
|---|---|---|---|---|
| Milligan-Morgan (Open) Hemorrhoidectomy | Excision of hemorrhoids with ligation of pedicle | Grade III-IV, failed conservative treatment | Definitive, low recurrence | Painful, longer recovery |
| Ferguson (Closed) Hemorrhoidectomy | Excision with primary closure | Grade III-IV hemorrhoids | Less pain, faster healing | Technical difficulty, hematoma risk |
| Stapled Hemorrhoidopexy (PPH) | Circular stapler to resect mucosa and reposition hemorrhoids | Grade III-IV circumferential hemorrhoids | Less pain, faster recovery | Cost, rare serious complications |
| Doppler-guided Hemorrhoidal Artery Ligation (HAL) | Ligation of hemorrhoidal arteries under Doppler guidance | Grade II-III hemorrhoids | Minimal pain, minimal tissue damage | Special equipment, higher recurrence |
Treatment Algorithm According to Love & Bailey
| Grade | First-line | Second-line | Third-line |
|---|---|---|---|
| I | Diet, lifestyle, topical treatments | Banding, sclerotherapy | Infrared coagulation |
| II | Diet, lifestyle, banding | Sclerotherapy, infrared coagulation | Hemorrhoidectomy if persistent |
| III | Banding, hemorrhoidectomy | Stapled hemorrhoidopexy | HAL-RAR |
| IV | Hemorrhoidectomy | Stapled hemorrhoidopexy | Combined procedures |
Complications of Hemorrhoids and Their Treatment
Complications of Hemorrhoidal Disease
| Complication | Incidence | Management |
|---|---|---|
| Anemia | 0.5-1% of patients | Iron supplementation, definitive treatment of hemorrhoids |
| Strangulation | 2-3% of prolapsed hemorrhoids | Emergency hemorrhoidectomy |
| Thrombosis | 5-10% of external hemorrhoids | Evacuation if early, conservative if late |
| Gangrene | Rare | Emergency surgery, antibiotics |
| Fibrosis/Stenosis | Chronic cases | Dilatation, surgery |
Complications of Surgical Treatment
| Complication | Incidence | Prevention | Management |
|---|---|---|---|
| Pain | Common (especially open hemorrhoidectomy) | Multimodal analgesia, topical treatments | Analgesics, sitz baths |
| Bleeding | 1-2% (primary), 0.5-1% (secondary) | Meticulous technique, secure pedicle ligation | Pressure, suture ligation, packing |
| Urinary Retention | 10-15% | Adequate hydration, limited IV fluids, pain control | Catheterization if persistent |
| Infection | 0.5-1% | Aseptic technique, perioperative antibiotics if indicated | Antibiotics, drainage if abscess |
| Anal Stenosis | 1-2% | Preserve mucosal bridges, avoid excessive excision | Dilatation, anoplasty |
| Incontinence | Rare (0.5%) | Careful surgical technique, preserve sphincters | Biofeedback, surgical repair if severe |
Special Considerations
Hemorrhoids in Immunocompromised Patients
Avoid invasive procedures if possible
Higher risk of infection and poor healing
Conservative management preferred
If surgery needed, meticulous technique and antibiotic prophylaxis
Hemorrhoids in Inflammatory Bowel Disease
Conservative management preferred
Surgery only for severe symptoms
Risk of poor healing and fistula formation
Coordinate care with gastroenterologist
Recurrent Hemorrhoids
Evaluate for underlying causes (chronic constipation, etc.)
Consider alternative procedures
May require re-do hemorrhoidectomy
Assess sphincter function preoperatively
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Anorectal Diseases in Love & Bailey’s textbook
American Society of Colon and Rectal Surgeons Clinical Practice Guidelines
Association of Coloproctology of Great Britain and Ireland Guidelines
World Society of Emergency Surgery Guidelines
Key Learning Points from Love & Bailey
“Hemorrhoids are a common condition that can usually be managed conservatively. Surgical intervention should be reserved for cases that fail conservative measures or present with complications. A thorough understanding of anal anatomy is essential for safe and effective treatment.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Never attribute rectal bleeding to hemorrhoids without proper examination
Pain is not a typical feature of uncomplicated internal hemorrhoids
Conservative management should always be tried first
Always consider and exclude other causes of rectal bleeding
Patient education about bowel habits is crucial for prevention
Surgical treatment should be tailored to the grade of hemorrhoids and patient factors
Postoperative pain management is essential for patient satisfaction
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog