· Mayank Kashyap · 6 min read
Breast Surgery
According to Love and Bailey's "A Short Practice of Surgery", shock is defined as a state of circulatory inadequacy with impaired tissue perfusion leading to cellular hypoxia and dysfunction.
Introduction to Breast Diseases
According to Love and Bailey’s “A Short Practice of Surgery”, breast diseases represent a significant portion of surgical practice, ranging from benign conditions to malignant tumors that are among the most common cancers in women.
Epidemiological Significance
Breast cancer is the most common cancer in women worldwide
Approximately 1 in 8 women will develop breast cancer during their lifetime
Benign breast conditions are even more common than malignant ones
Proper differentiation between benign and malignant conditions is crucial
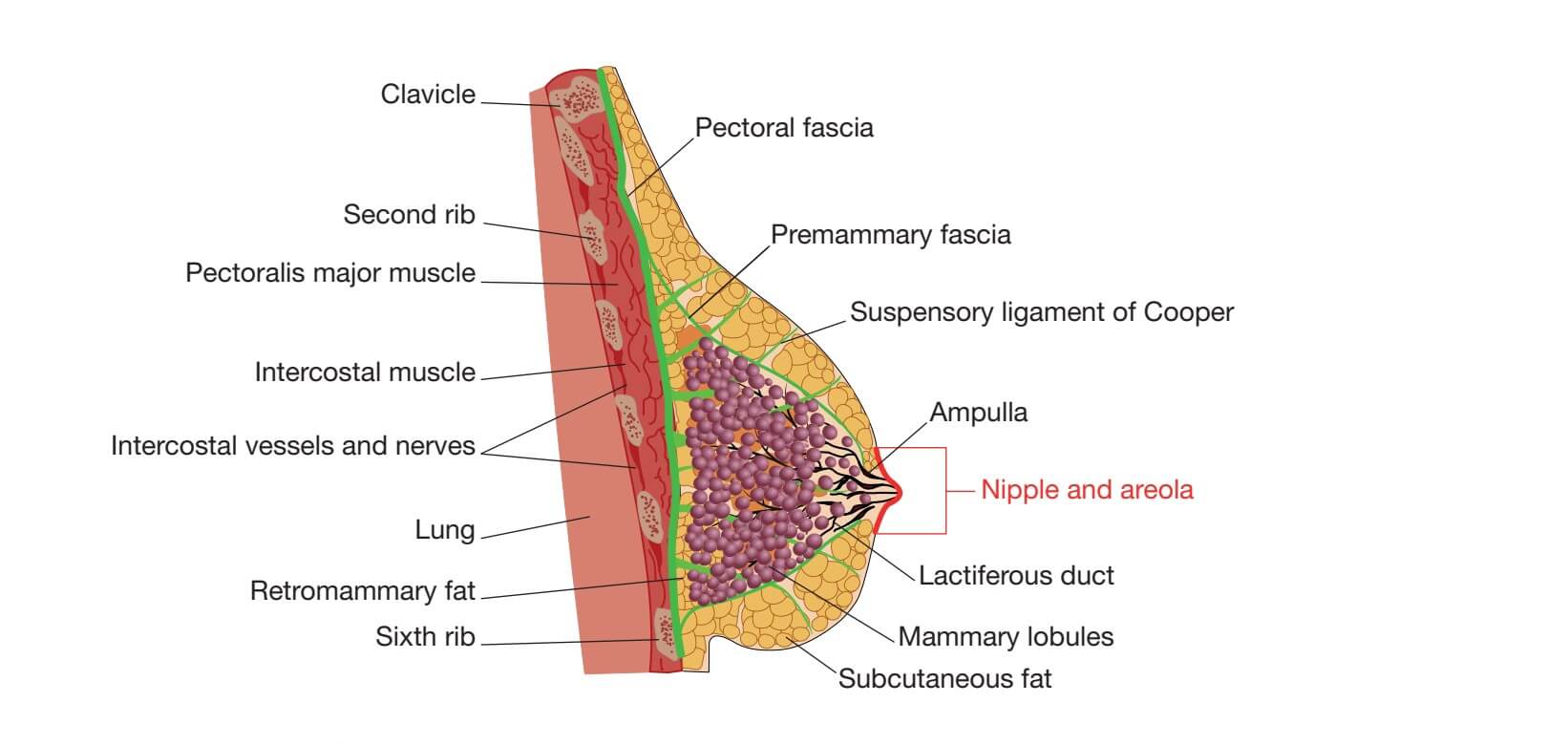
Breast Anatomy and Physiology
Anatomical Structure
Parenchyma: 15-20 lobes arranged radially
Lobules: Functional units that produce milk
Ducts: Transport milk to nipple
Stroma: Fatty and connective tissue providing support
Blood Supply: Mainly from internal mammary and lateral thoracic arteries
Lymphatic Drainage: 75% to axillary nodes, 25% to internal mammary chain
Physiological Changes
Development during puberty under hormonal influence
Cyclical changes during menstrual cycle
Pregnancy-induced hyperplasia and differentiation
Involution during menopause
Benign Breast Tumors and Conditions
Classification of Benign Breast Diseases
| Condition | Age Group | Clinical Features | Pathology |
|---|---|---|---|
| Fibroadenoma | 15-35 years | Firm, mobile, painless mass (“breast mouse”) | Epithelial and stromal proliferation |
| Fibrocystic Disease | 30-50 years | Painful, lumpy breasts, cyclical symptoms | Cysts, fibrosis, adenosis |
| Intraductal Papilloma | 35-55 years | Bloody nipple discharge, subareolar mass | Papillary growth in lactiferous duct |
| Phyllodes Tumor | 40-50 years | Rapidly growing, large, mobile mass | Biphasic tumor with leaf-like pattern |
| Mastitis/Abscess | Lactating women | Pain, erythema, fever, fluctuant mass | Inflammation/infection of breast tissue |
| Duct Ectasia | Perimenopausal | Greenish nipple discharge, periareolar mass | Dilatation of subareolar ducts |
Detailed Description of Common Benign Conditions
Fibroadenoma
According to Love and Bailey, fibroadenomas are the most common benign breast tumors in young women.
Pathogenesis: Hormonally responsive localized overgrowth of stromal and epithelial elements
Clinical Features:
Well-circumscribed, firm, rubbery mass
Highly mobile (“breast mouse”)
Usually painless
Size may vary with menstrual cycle
Management:
Observation if small and asymptomatic
Excision if large, growing, or causing anxiety
Vacuum-assisted excision for selected cases
Fibrocystic Disease (Fibrocystic Change)
A spectrum of benign changes rather than a true disease entity.
Types:
Non-proliferative changes (cysts, fibrosis)
Proliferative changes without atypia
Atypical hyperplasia (increased cancer risk)
Clinical Features:
Breast pain (mastalgia), worse premenstrually
Multiple bilateral lumps
Nodularity and thickening
Management:
Reassurance and supportive measures
Analgesics for pain
Hormonal therapy in severe cases
Aspiration of symptomatic cysts
Phyllodes Tumor
Rare fibroepithelial tumors with potential for local recurrence.
Classification: Benign, borderline, malignant
Clinical Features: Rapid growth, large size, smooth surface
Treatment: Wide local excision with clear margins
Prognosis: Good for benign types, variable for malignant
Breast Cancer
Risk Factors for Breast Cancer
| Risk Factor | Relative Risk | Remarks |
|---|---|---|
| Female gender | 100x | Male breast cancer accounts for <1% |
| Increasing age | 3-4x | Risk increases with age, peak at 60-70 years |
| Family history | 2-4x | Especially first-degree relatives |
| BRCA1/BRCA2 mutation | 5-20x | High lifetime risk, earlier onset |
| Early menarche (<12 years) | 1.5-2x | Longer lifetime estrogen exposure |
| Late menopause (>55 years) | 1.5-2x | Longer lifetime estrogen exposure |
| Nulliparity | 1.5x | Protective effect of early pregnancy |
| Hormone replacement therapy | 1.2-1.7x | Combined estrogen-progestin increases risk |
| Previous breast biopsy | 1.5-2x | Especially with atypical hyperplasia |
Pathological Classification of Breast Cancer
Non-invasive Breast Cancer
Ductal Carcinoma In Situ (DCIS):
Malignant cells confined to ducts
No invasion through basement membrane
Considered a precursor to invasive cancer
Often detected mammographically as microcalcifications
Lobular Carcinoma In Situ (LCIS):
Not a true cancer but a marker for increased risk
Bilateral multifocal disease common
Management typically involves close surveillance
Invasive Breast Cancer
| Type | Frequency | Characteristics | Prognosis |
|---|---|---|---|
| Invasive Ductal Carcinoma (NOS) | 70-80% | No special features, most common type | Variable, depends on grade and stage |
| Invasive Lobular Carcinoma | 5-15% | Single file growth pattern, often multifocal | Similar to ductal when matched for stage |
| Tubular Carcinoma | 1-2% | Well-differentiated, orderly tubular structures | Excellent |
| Mucinous (Colloid) Carcinoma | 1-2% | Abundant extracellular mucin, elderly patients | Favorable |
| Medullary Carcinoma | 1-2% | Pushing margins, lymphocytic infiltrate | Better than expected for grade |
| Inflammatory Carcinoma | 1-3% | Dermal lymphatic invasion, erythema, edema | Poor, advanced at presentation |
Clinical Presentation of Breast Cancer
Palpable mass: Most common presentation (80-90%)
Nipple changes: Retraction, discharge, Paget’s disease
Skin changes: Dimpling (peau d’orange), erythema, ulceration
Axillary mass: Lymph node metastasis
Asymptomatic: Detected by screening mammography
Advanced disease: Bone pain, weight loss, respiratory symptoms
Staging of Breast Cancer (TNM System)
| Stage | Tumor (T) | Nodes (N) | Metastasis (M) | 5-Year Survival |
|---|---|---|---|---|
| 0 | Tis (DCIS/LCIS) | N0 | M0 | ~100% |
| I | T1 (≤2 cm) | N0 | M0 | ~95% |
| IIA | T0-1 | N1 | M0 | ~85% |
| IIB | T2-3 | N0 | M0 | ~80% |
| IIIA | T0-2 | N2 | M0 | ~65% |
| IIIB | T4 | Any N | M0 | ~45% |
| IIIC | Any T | N3 | M0 | ~35% |
| IV | Any T | Any N | M1 | ~20% |
Diagnosis of Breast Diseases
Triple Assessment Approach
According to Love and Bailey, the diagnosis of breast diseases relies on the triple assessment method:
Clinical Assessment:
Thorough history and physical examination
Inspection for symmetry, skin changes, nipple abnormalities
Palpation of breasts and regional lymph nodes
Imaging:
Mammography: Gold standard for screening, especially in women >40 years
Ultrasound: Useful for characterizing masses, guiding procedures, in young women
MRI: High sensitivity, used for high-risk screening, implant evaluation, staging
Pathology:
Fine Needle Aspiration Cytology (FNAC): Quick, minimally invasive, high accuracy
Core Needle Biopsy: Provides tissue architecture, hormone receptor status
Excision Biopsy: Definitive diagnostic and therapeutic procedure
Breast Imaging Reporting and Data System (BI-RADS)
| BI-RADS Category | Assessment | Recommended Action |
|---|---|---|
| 0 | Incomplete | Need additional imaging |
| 1 | Negative | Routine screening |
| 2 | Benign | Routine screening |
| 3 | Probably benign | Short-term follow-up (6 months) |
| 4 | Suspicious | Biopsy recommended |
| 5 | Highly suggestive of malignancy | Appropriate action (biopsy) |
| 6 | Known biopsy-proven malignancy | Appropriate action (treatment) |
Treatment of Breast Cancer
Surgical Management
| Procedure | Indications | Advantages | Disadvantages |
|---|---|---|---|
| Breast Conservation Therapy (Lumpectomy + Radiation) | Early stage, small tumors, favorable location | Preserves breast, better cosmesis, equivalent survival to mastectomy | Requires radiation therapy, possible local recurrence |
| Modified Radical Mastectomy | Large tumors, multifocal disease, patient preference | Single procedure, lower local recurrence rate | Breast loss, body image issues |
| Sentinel Lymph Node Biopsy | Clinically node-negative patients | Less morbidity than axillary dissection, accurate staging | False negative rate, learning curve |
| Axillary Lymph Node Dissection | Positive sentinel nodes, clinically positive axilla | Good regional control, accurate staging | Lymphedema, shoulder dysfunction, nerve injury |
Adjuvant Systemic Therapy
Chemotherapy
Indications: Node-positive disease, high-risk node-negative, large tumors, aggressive subtypes
Common Regimens: Anthracycline-based (AC, FAC), taxane-based, CMF
Neoadjuvant Chemotherapy: Administered before surgery to downstage tumors, assess response
Endocrine Therapy
Indications: Hormone receptor-positive tumors (ER+ and/or PR+)
Agents:
Tamoxifen: Selective estrogen receptor modulator, used in pre- and postmenopausal women
Aromatase Inhibitors: Anastrozole, letrozole, exemestane (postmenopausal only)
Ovarian Suppression: GnRH agonists in premenopausal women
Duration: Typically 5-10 years
Targeted Therapy
HER2-targeted Therapy: Trastuzumab, pertuzumab, T-DM1 for HER2-positive tumors
CDK4/6 Inhibitors: Palbociclib, ribociclib, abemaciclib for HR+/HER2- advanced disease
PARP Inhibitors: Olaparib, talazoparib for BRCA-mutated tumors
Radiation Therapy
Indications: After breast conservation, positive margins, extensive nodal involvement
Techniques: Whole breast irradiation, accelerated partial breast irradiation, boost to tumor bed
Duration: Typically 3-6 weeks
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Breast Diseases in Love & Bailey’s textbook
National Comprehensive Cancer Network (NCCN) Guidelines
American Society of Clinical Oncology (ASCO) Guidelines
European Society for Medical Oncology (ESMO) Guidelines
Key Learning Points from Love & Bailey
“The management of breast diseases requires a multidisciplinary approach with careful clinical assessment, appropriate imaging, and histological confirmation. Early detection and treatment of breast cancer significantly improve outcomes.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Triple assessment is the cornerstone of breast disease diagnosis
Most breast lumps are benign, but all require proper evaluation
Breast conservation therapy provides equivalent survival to mastectomy for early-stage cancer
Sentinel lymph node biopsy has revolutionized axillary staging
Molecular subtyping guides targeted therapy decisions
Regular screening mammography reduces breast cancer mortality
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
Breast is modified sweat gland.
Located between 2nd to 6th rib.
Lymphatic drainage 85-90% by axillary group of lymph nodes and 10-15% by internal mammary lymph nodes.
For assessment of breast lump :- Triple assessment, which include Radiological investigation + Clinical Examination + Histopathological Examination
Radiological investigation for less 40 years USG is recommended because (glands>fat) whereas for more than 40 years of age mammogram is recommended because (fat>glands).
Breast imaging reporting and data system(BIRADS).
Breast cancer 10% is familiar while 90% is sporadic.
ANDI(Aberration of Normal Development and Involution).
In age group 15-25 years Fibroadenoma is common which is a benign tumor of breast.