· Mayank Kashyap · 5 min read
Acute pancreatitis
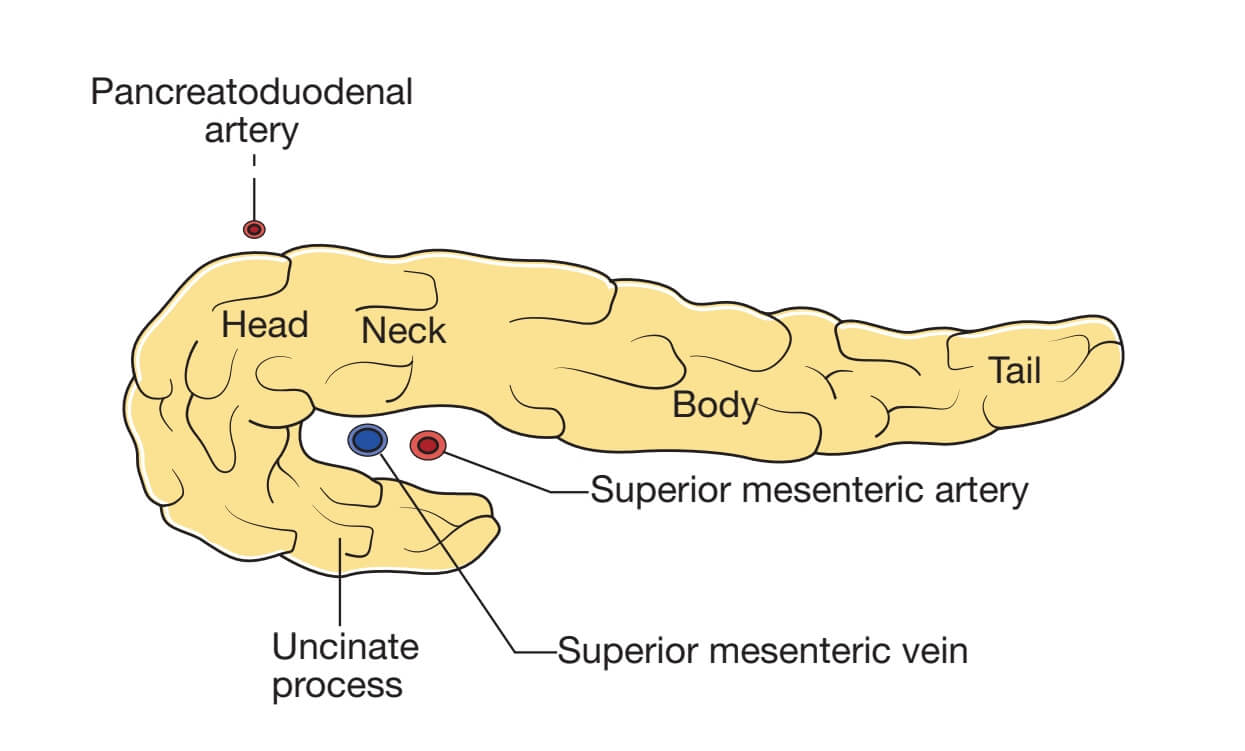
According to Love and Bailey's "A Short Practice of Surgery", acute pancreatitis is defined as an acute inflammatory condition of the pancreas with varying involvement of other regional tissues or remote organ systems.
Introduction to Acute Pancreatitis
According to Love and Bailey’s “A Short Practice of Surgery”, acute pancreatitis is defined as an acute inflammatory condition of the pancreas with varying involvement of other regional tissues or remote organ systems.
Key Epidemiological Facts
Incidence: 5-80 cases per 100,000 population annually
Mild edematous pancreatitis accounts for 80% of cases
Severe necrotizing pancreatitis occurs in 20% of cases
Overall mortality: 5-10% (higher in severe cases)
Etiology and Risk Factors
Common Causes (According to Love & Bailey)
| Etiology | Frequency | Remarks |
|---|---|---|
| Gallstones | 40-50% | Most common cause worldwide. |
| Alcohol | 25-35% | More common in males, chronic consumption. |
| Idiopathic | 10-20% | No identifiable cause after investigation. |
| Hypertriglyceridemia | 1-4% | Triglycerides >1000 mg/dL |
| ERCP-induced | 3-5% | Iatrogenic, usually mild. |
| Drug-induced | 1-2% | Azathioprine, thiazides, steroids, etc. |
| Trauma | 1-2% | Blunt abdominal trauma, surgical injury. |
Less Common Causes
Infections (mumps, coxsackievirus, CMV)
Autoimmune pancreatitis
Hypercalcemia
Pancreatic duct obstruction
Hereditary pancreatitis
Scorpion venom (Tityus trinitatis)
Pathophysiology
Key Mechanisms According to Love & Bailey
1. Autodigestion Theory
The fundamental pathological process involves premature activation of pancreatic enzymes within the pancreas itself:
Trypsinogen → Trypsin (key activating enzyme)
Activation of other proenzymes (phospholipase A2, elastase)
Digestion of pancreatic parenchyma and peripancreatic tissues
Release of inflammatory mediators
2. Inflammatory Cascade
Activation of complement system
Release of cytokines (TNF-α, IL-1, IL-6, IL-8)
Activation of coagulation system
Systemic inflammatory response syndrome (SIRS)
3. Gallstone Pathogenesis
“Common channel” hypothesis:
Gallstone impacts at ampulla of Vater
Obstruction of pancreatic duct
Increased intraductal pressure
Activation of pancreatic enzymes
Pancreatic injury and inflammation
Clinical Features
Cardinal Symptoms
Abdominal pain: Severe, constant, epigastric radiating to back
Nausea and vomiting: Profuse, not relieving pain
Fever: Low-grade in mild cases, high in severe cases
Abdominal distension: Due to ileus
Physical Examination Findings
| Finding | Description | Significance |
|---|---|---|
| Abdominal tenderness | Epigastric with guarding | Localized or generalized peritonitis |
| Cullen’s sign | Periumbilical bruising | Indicates hemorrhagic pancreatitis |
| Grey Turner’s sign | Flank bruising | Indicates hemorrhagic pancreatitis |
| Hypotension | Systolic BP <90 mmHg | Severe pancreatitis with third spacing |
| Tachycardia | Heart rate >100/min | Systemic inflammatory response |
| Tachypnea | Respiratory rate >20/min | Pleural effusion or ARDS |
Diagnosis and Investigations
Diagnostic Criteria (Atlanta Classification)
Requires at least 2 of the following 3 features:
Abdominal pain consistent with acute pancreatitis
Serum amylase or lipase >3 times upper limit of normal
Characteristic findings on imaging (CT, MRI, or US)
Laboratory Investigations
| Test | Findings | Clinical Significance |
|---|---|---|
| Serum amylase | Elevated (>3× normal) | Rises in 2-12 hours, normalizes in 3-5 days |
| Serum lipase | Elevated (>3× normal) | More specific, remains elevated longer |
| Complete blood count | Leukocytosis | Marked elevation in severe cases |
| Liver function tests | Elevated bilirubin/ALP | Suggests gallstone etiology |
| Serum calcium | Hypocalcemia | Prognostic marker, indicates severity |
| CRP | Elevated | Best laboratory marker of severity |
Imaging Studies
Abdominal ultrasound: First-line for detecting gallstones, assessing biliary tree
Contrast-enhanced CT: Gold standard for diagnosis and assessing severity
MRI/MRCP: Excellent for detecting ductal abnormalities, subtle necrosis
Endoscopic ultrasound: For detecting microlithiasis, tumors
Severity Assessment
Ranson’s Criteria (at admission and 48 hours)
| At Admission | During Initial 48 Hours |
|---|---|
| Age >55 years | Hct decrease >10% |
| WBC >16,000/mm³ | BUN increase >5 mg/dL |
| Blood glucose >200 mg/dL | Serum calcium <8 mg/dL |
| LDH >350 IU/L | Arterial PO₂ <60 mmHg |
| AST >250 IU/L | Base deficit >4 mEq/L |
| Fluid sequestration >6 L |
Interpretation: Mortality: 0-2 criteria = 2%, 3-4 criteria = 15%, 5-6 criteria = 40%, >6 criteria = 100%
Management Principles
Initial Management (According to Love & Bailey)
Resuscitation:
Aggressive IV fluid therapy (crystalloids)
Monitor urine output (target >0.5 mL/kg/hr)
Correct electrolyte abnormalities
Pain Management:
Opioids (preferably patient-controlled analgesia)
Avoid morphine (may cause sphincter of Oddi spasm)
Nutritional Support:
Mild cases: NPO initially, advance as tolerated
Severe cases: Enteral nutrition (nasojejunal preferred)
Parenteral nutrition if enteral route not feasible
Monitoring:
Vital signs, fluid balance, organ function
Serial clinical assessment and laboratory tests
Specific Treatments
Gallstone Pancreatitis
Early ERCP (within 72 hours) for cholangitis or persistent biliary obstruction
Cholecystectomy during same admission for mild cases
Delayed cholecystectomy (after resolution) for severe cases
Severe Acute Pancreatitis
ICU admission for monitoring and organ support
Antibiotics for infected necrosis (proven or suspected)
Minimally invasive or open necrosectomy for infected necrosis not responding to antibiotics
Complications of Acute Pancreatitis
Local Complications
| Complication | Timing | Management |
|---|---|---|
| Acute peripancreatic fluid collection | <4 weeks | Conservative, drainage if symptomatic |
| Pancreatic pseudocyst | >4 weeks | Drainage if >6cm or symptomatic |
| Acute necrotic collection | <4 weeks | Antibiotics if infected, drainage |
| Walled-off necrosis | >4 weeks | Drainage if infected or symptomatic |
| Pancreatic abscess | >4 weeks | Percutaneous or surgical drainage |
Systemic Complications
Respiratory: Pleural effusion, ARDS, atelectasis
Cardiovascular: Hypotension, arrhythmias, myocardial depression
Renal: Acute kidney injury, renal failure
Hematological: DIC, thrombocytopenia
Metabolic: Hypocalcemia, hyperglycemia, hypertriglyceridemia
Gastrointestinal: Ileus, portal vein thrombosis, colonic necrosis
References
Love, R. J. M., & Bailey, H. (Latest Edition). A Short Practice of Surgery. London: Edward Arnold.
Chapter on Pancreatic Diseases in Love & Bailey’s textbook
American Gastroenterological Association Guidelines on Acute Pancreatitis
International Association of Pancreatology Guidelines
Atlanta Classification of Acute Pancreatitis (Revised)
Key Learning Points from Love & Bailey
“The management of acute pancreatitis requires a multidisciplinary approach with careful monitoring, aggressive fluid resuscitation, and timely intervention for complications.”
- Love & Bailey, A Short Practice of Surgery
Important Clinical Pearls
Early aggressive fluid resuscitation improves outcomes
Contrast-enhanced CT is the gold standard for diagnosis and staging
Enteral nutrition is preferred over parenteral nutrition
Infected pancreatic necrosis requires drainage and/or debridement
Cholecystectomy should be performed during the same admission for gallstone pancreatitis
This educational blog is based on the surgical textbook “A Short Practice of Surgery” by Love and Bailey.
For medical professionals and students only. Always consult current guidelines and local protocols.
© Medical Education Blog
Most common cause of acute pancreatitis is gall stones.
2nd most common cause is alcohol.
Other cause include Secondary to trauma.
Iatrogenic causes e.g. post-ERCP(Endoscopic Retrograde CholangioPancreaticography).
Pathogenesis is Explained by Co-localisation theory, In which enzymes of pancreas activate inside it and start causing damage to pancreas.
Clinical features include pain in epigastric region, which relieves on bending.
Signs include grey turner sign, cullen sign and fox sign.
Diagnostic criteria involves any 2 positive out of imaging suggestive, three fold rise in serum amylase and pain in right epigastric region associated with acute pancreatitis.
Investigation of choice is (CECT)Contrast Enhanced Computed Tomography.
For chronic pancreatitis there is TIGARO classification where T stands for Toxins, I stands for Idiopathic, G stands for Genetic, A stands for Autoimmune, R stands for Recurrent, O stands for Obstructive.
Investigation of choice is MRCP.